Cartilage Repair Techniques
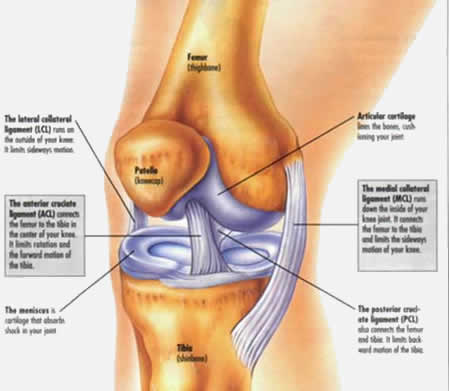
Articular (hyaline) cartilage lines the ends of bones within a joint. It is a complex structure which provides almost frictionless movement of a normal joint.
 Once damaged, articular cartilage has no ability to repair itself. If damaged cartilage is left, the defect circumference will eventually increase to become osteoarthritis. Repairing the cartilage that lines the joint as soon as possible is likely to delay or stop the onset of arthritis.
Once damaged, articular cartilage has no ability to repair itself. If damaged cartilage is left, the defect circumference will eventually increase to become osteoarthritis. Repairing the cartilage that lines the joint as soon as possible is likely to delay or stop the onset of arthritis.
As with most soft tissue knee injuries, cartilage damage is caused by twisting the knee usually during sports such as football, rugby or hockey.
The smooth cartilage is gouged out leaving a defect. (also known as an osteo-chondral defect )
(its rather like a taking divot of turf when playing a golf shot)
Symptoms
- Localised pain
- Swelling
- Giving way
- Locking of the knee
Diagnosis can be made by X-ray (Schuss view) but usually the defect is more accurately seen with an MRI scan.
It is very difficult to replicate the complex structure and function of articular cartilage once damaged.
Various techniques have been described. Below are listed the treatments which I offer. Bear in mind that each defect is different and I will tailor the appropriate treatment to you.
- 1. Micro-fracture
After carefully preparing the site of cartilage loss, 2mm holes are created in the bony base of the defect. This allows stem cells from your bone marrow to fill the defect. This “super-clot” then has the ability to transform itself into fibro-cartilage over the course of 6-8 weeks, thus filling the defect.
Rehabilitation Guidelines Following Microfracture Procedures to the Knee Information Booklet

Creating the 2mm holes using a special instrument
Advantages: Technically easy, arthroscopic procedure
Disadvantages: Fibrocartilage does not have the same properties as hyaline cartilage so could wear long term, the fill of the defect is not certain
- 2. Osteo-chondral transfer
In this procedure, I take cylinders of hyaline cartilage and bone from a non-weight bearing area of the knee and transfer these into the carefully prepared defect.

Advantages: The defect is covered immediately with stable, hyaline cartilage.
Disadvantages: Open procedure (10cm incision to the inner aspect of kneecap), some question mark over the donor site long term
- 3. Maoiregen TM
In this procedure, I first perform a micro fracture followed by insertion a biological scaffold into the defect. The scaffold is made of 3 layers and ensures that the stem cells in the “super-clot” stay in the defect and form cartilage which is closer in structure to hyaline cartilage when compared to fibrocartilage.

Diagram showing the structure of the scaffold


Diagram showing how the scaffold is inserted
Advantages: No donor site problems, higher rate of filling the defect compared with micro-fracture alone, good for filing larger defects
Disadvantages: Open procedure (5cm incision to the inner aspect of kneecap), no long term studies of functional outcome yet
